The Lamen
THE MOST COMMON COMPLICATIONS OF DIABETES
Chronically high blood sugar levels can lead to a range of type 2 diabetes complications, including cardiovascular disease, erectile dysfunction, and dementia, that can cause serious damage to your body.
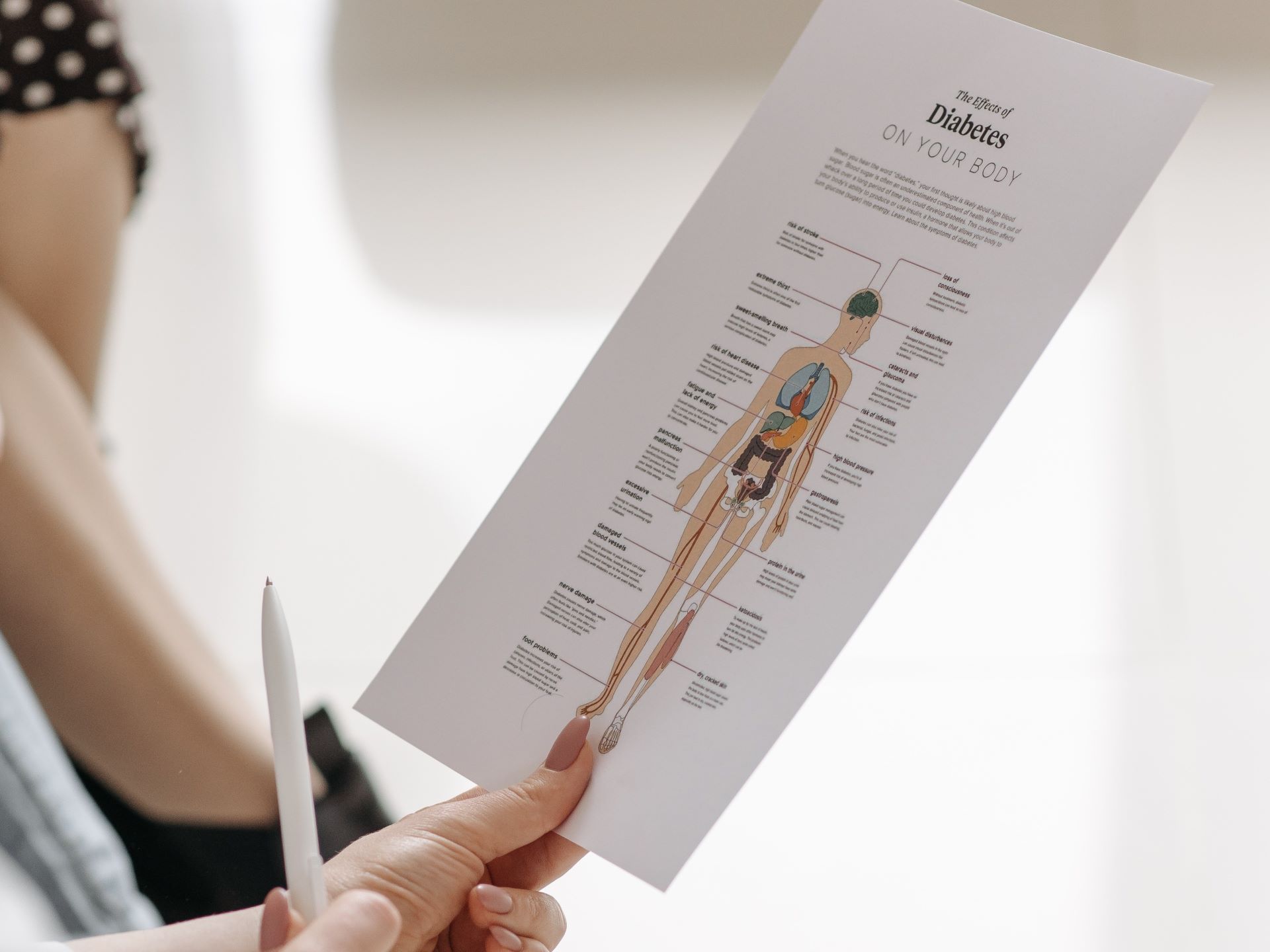
Image: Pexels
Type 2 diabetes has become one of the biggest chronic public health problems. Additionally, most people with T2D experience at least one complication.
There are 2 types of complications of diabetes that a person might experience: acute and chronic.
Acute complications are typically short-term that can happen at any time, which may lead to long-term complications. Chronic complications, on the other hand, are complications that develop gradually and may lead to series issues.
SHORT-TERM COMPLICATIONS
Acute (short-term) complications of type 2 diabetes like diabetic ketoacidosis (DKA), hyperglycemic hyperosmolar state (HHS), and hypoglycemia can be potential life threatening.
HYPOGLYCEMIA
Hypoglycemia occurs when your blood sugar levels drop below the healthy range. For most people with diabetes, hypoglycemia happens when their blood sugar levels drop below 70 mg/dL (or 4 mmol/l).
Hypoglycemia is one of the most common short-term complications of type 2 diabetes.
The symptoms of low blood sugar include:
- feeling hungry and tired
- feeling dizzy, lightheaded, confused, or irritable
- nausea or headache
- feeling shaky
- blurred vision
- night sweats
Severe hypoglycemia may even lead to losing consciousness or having a seizure.
Hypoglycemia should be treated immediately, typically by eating 15 to 20 grams of a fast-acting carbohydrate like glucose, fruit juice, or a candy with sugar.
Follow it up by testing your blood sugar 15 minutes later. If your blood sugar levels are not back above 70 mg/dL, had some more fast acting carbs, and retest after 15 minutes.
Once things are back to normal, have a normal meal to prevent the condition from recurring. If someone experiences severe hypoglycemia, they should receive medical attention immediately.
HYPERGLYCEMIA
Hyperglycemia happens when your blood sugar is too high.
A person has hyperglycemia if they have a blood glucose of more than 125 mg/dL while fasting for at least 8 hours, or more than 180 mg/dL 2 hours after a meal.
Symptoms of hyperglycemia include:
- frequent urination, especially at night
- thirst
- blurred vision
- feeling sick
People with diabetes typically manage hyperglycemia by injecting insulin, the dosage of which varies based on several factors.
For T2D patients who don’t require insulin, they can manage hyperglycemia with dietary changes and exercise.
If hyperglycemia is left untreated, it can lead to a life threating condition called diabetic ketoacidosis (DKA).
HYPEROSMOLAR HYPERGLYCEMIC STATE (HHS)
Hyperosmolar hyperglycemic state is a life-threatening complication of diabetes. It occurs when your blood sugar levels are too high, but no ketones are present.
The mortality rate of HHS can be as high as 20 percent, which is about 10 times greater than the mortality rate of diabetic ketoacidosis.
Symptoms of HHS can take from days or weeks to develop and include:
- very high blood sugar levels (over 600 mg/dL)
- vision loss
- hallucinations
- extreme thirst
- frequent urination
Infections are the leading cause of HHS, accounting for nearly 60 percent of all cases. The most commonly linked infections include pneumonia, sepsis, dental infections, and urinary tract infections.
Treatment of hyperosmolar hyperglycemic state requires immediate medical attention, where the healthcare provider provides you fluids, electrolytes, and insulin.
DIABETIC KETOACIDOSIS
Diabetic ketoacidosis, also called ketoacidosis, is a potentially life-threatening complication of diabetes.
Ketoacidosis occurs when your body severely lacks insulin, which means that it can’t process sugars to produce energy. Instead, your body starts breaking down fats.
This results in the formation of ketones – which can slowly accumulate in your body, eventually moving to the blood. This buildup makes your blood acidic.
Early symptoms of ketoacidosis include:
- a very dry mouth
- frequent urination
- fruity odor on breath
The condition can become life-threatening in just a few hours, with symptoms including:
- dry or flushed skin
- abdominal pain
- nausea or vomiting
- difficulty breathing
Diabetic ketoacidosis is a medical emergency that needs to be treated immediately.
DIARRHEA FROM MEDICATIONS
Diabetes-related diarrhea is a common condition and is typically caused by diabetes medication such as metformin.
According to a study published by the American Diabetes Association (ADA), gastrointestinal side effects such as diarrhea occur in up to 75 percent of people who take metformin.
Other such side effects include:
- nausea or vomiting
- flatulence
- abdominal discomfort
- anorexia
Metformin-induced diarrhea in individuals who have just started taking the medication has been linked with changes in the gut microbiome and increased intestinal glucose.
The condition usually subsides with time or after a reduction in dosage.
Besides medications, diabetes-related diarrhea might also be caused by autonomic neuropathy (nerve damage), IBS, or overconsumption of artificial sweeteners.
LONG-TERM TYPE 2 DIABETES COMPLICATIONS
The long-term complications of diabetes can take years to develop and can be attributed to how chronically high blood sugar levels affect your body over time.
VISION PROBLEMS
Chronically high blood sugar levels can damage the tiny blood vessels in your eyes. While this damage can begin during prediabetes, you are not likely to experience anything in the short term.
Over time, you can develop serious eye conditions like:
- diabetic retinopathy, when damaged blood vessels cause damage to your retina
- glaucoma, when fluid builds up in the front part of your eye
- diabetic macular edema, caused by the accumulation of excess fluid in your eye
- cataract, or cloudy vision
Diabetic retinopathy is the most common cause of diabetes-related vision loss. An estimated one in three people over 40 with diabetes already show some signs of diabetic retinopathy.
Symptoms of diabetes-related eye disease typically appear after some time. These include:
- blurry vision
- dark spots or areas in the vision
- flashes of light
- complete loss of sight
If you have been diagnosed with diabetes and are experiencing vision problems, you should seek a medical diagnosis.
According to the ADA, a routine annual eye examination can prevent up to 95 percent of all vision loss caused by diabetes.
NERVE DAMAGE (NEUROPATHY)
Diabetic neuropathy describes nerve damage that occurs from diabetes – impacting different parts of the body.
There are different types of diabetic neuropathies, including:
- Peripheral neuropathy. It is the most common form of diabetic neuropathy, affecting the arms, hands, legs, and feet.
- Autonomic neuropathy. It affects the autonomic nervous system, which controls the involuntary systems of the body. This causes gastroparesis (digestive issues), irregular heartbeats, loss of bladder control, and impotence.
- Sensory neuropathy. Causes damage to the sensory nerves, affecting smell, taste, and feel.
- Thoracic/lumbar radiculopathy. This damages nerves in the thoracic area (torso) of the spine. It may cause shooting chest pain.
- Motor neuropathy. It affects the nerves that control movement, leading to muscle weakness and loss of coordination.
Controlling your blood sugar levels is the best way to prevent or delay diabetes-related nerve damage. Diabetes neuropathy currently has no known cure.
CARDIOVASCULAR DISEASE
Compared to individuals without diabetes, patients with type 2 diabetes have a considerably higher risk of developing cardiovascular disease. In fact, this risk could be up to twice to three times higher for people with diabetes.
High blood sugar levels can damage your arteries over time. People with diabetes are also more likely to experience high blood pressure, high triglycerides, and high LDL (bad) cholesterol levels.
If you have type 2 diabetes, taking the following steps can help lower your risk of CVD:
- lose weight and lower body fat
- eat a nutrient-dense, high-fiber diet
- exercise regularly
- monitor your blood pressure levels
- manage stress
Other factors that can influence the risk of cardiovascular disease include cigarette smoking, genetics, and dyslipidemia.
STROKE
A stroke occurs when blood flow to the brain is blocked, starving it of oxygen and other vital nutrients. Without oxygen, your brain cells begin to die within minutes, and can even lead to permanent damage or even death.
People with type 2 diabetes are twice as likely to have a stroke compared to those without, according to the American Stroke Association. They also tend to have a stroke at an earlier age.
Besides T2D, other factors that might increase the risk of a stroke include:
- high belly fat (obesity)
- high cholesterol levels
- high blood pressure
- smoking
- hypertension
Getting into a healthier weight range, eating a healthier diet, physical activity, and monitoring your blood pressure and blood cholesterol levels are vital in reducing your risk of a stroke – especially if you have diabetes.
KIDNEY PROBLEMS
Nearly 1 in 3 adults with diabetes have chronic kidney disease (CKD). High blood sugar levels can damage the blood vessels and nephrons in your kidneys.
When your kidneys are damaged, they don’t filter blood efficiently, causing a buildup of waste in your body.
According to the National Kidney Foundation, only 10 percent of adults with kidney disease ever get diagnosed. The condition often shows no symptoms and is diagnosed with blood and urine tests.
If present, the symptoms of kidney disease include:
- weight gain and swollen ankles
- frequent urination, especially at night
- morning sickness
- paleness and anemia
For people with type 2 diabetes, the most common sign of kidney disease is the presence of albumin, a protein, in the urine.
Controlling your diabetes, managing blood pressure, and getting treated for any urinary tract infections (UTIs) are vital in preventing kidney failure.
TOOTH DECAY AND OTHER DENTAL PROBLEMS
Diabetes and chronically high blood sugar levels lead to a greater risk of cavities, gum disease, and other oral issues.
High blood sugar levels can increase the amount of glucose in your saliva – which can feed harmful bacteria to increase the risk of cavities, tooth decay, and gum disease.
Additionally, people with diabetes who smoke are up to 20 times more likely to develop thrush (fungal infection of the mouth) and periodontal (gum) disease compared to non-smokers.
If you’re diabetic, you should see a dentist every few months for regular checkups. If you’re already suffering from oral disease, your insulin dose and other medications might need to be adjusted.
FOOT PROBLEMS
Some people with diabetes may experience numbness or swelling in their feet. This happens because of diabetic neuropathy, or diabetes-related nerve damage. It restricts blood flow to the feet and toes, and can cause a range of complications.
Up to 50 percent of adults with diabetes may develop neuropathy at some point. The condition causes loss of sensation, which might cause cuts or blisters to go unnoticed, in addition to an increased risk of wounds getting infected.
The most common signs of diabetes-related foot problems include:
- pins and needles sensation
- swollen feet
- burning sensation
- loss of feeling in your feet or legs
- sores or wounds that don’t heal
If you notice any such problem, you should keep your weight off your feet and seek medical attention. If left untreated, a serious foot problem could require amputation.
SEXUAL ISSUES
Type 2 diabetes can cause sexual issues in both men and women, including lower sex drive, erectile dysfunction (ED), and increased risk of urinary tract infections.
Erectile dysfunction is considered the most important sexual problem in men with diabetes – nearly 3.5 times higher in men with diabetes compared to those without.
Diabetes can damage the blood vessels and nerves in your penis. Diabetes can also cause other complications that indirectly lead to erectile dysfunction, including hypertension, obstructive sleep apnea, and depression.
Another common side effect of diabetes is vaginal dryness, which happens due to damaged blood vessels in the vagina and lack of lubrication.
While you’re not likely to get an STI if you have diabetes, you are at a greater risk of developing other infections, such as fungal infections and UTIs.
DEMENTIA
While the most common signs of dementia are memory loss, confusion, and loss of thinking abilities, the condition is not simply a part of aging.
Researchers have found that type 2 diabetes is one of the strongest predictors of cognitive decline in older adults. In fact, a study found that the risk of experiencing cognitive decline over a 5-year period was almost double in older adults with diabetes.
While doctors don’t yet understand how dementia and diabetes are connected, we know that high blood sugar can harm the brain through damage to blood vessels and neurons, and through inflammation.
A strong correlation is also found between diabetes and Alzheimer’s disease.
CANCER
Researchers are still trying to understand the connection between type 2 diabetes and cancer, and current findings suggest that an estimated 20 percent of cancer patients already have diabetes.
Cancer patients with type 2 diabetes have been found more likely to die from the condition, and are also more likely to not respond well to treatment.
Some chemotherapy drugs and well as steroids can also lead to high blood sugar levels, which may lead to serious complications.
If you have diabetes and are at an increased risk of some form of cancer, you should get regular preventive screenings, along with managing your weight and blood sugar levels.
PREVENTING TYPE 2 DIABETES COMPLICATIONS
The first step in preventing the long-term complications of type 2 diabetes is making appropriate lifestyle changes.
- Get more exercise and lose weight.
- Make the necessary changes to your diet.
- Be proactive about your medications.
- Educate yourself.
- Cut back on alcohol and smoking.
According to the National Institutes of Health (NIH), people can follow the diabetes ABCS to manage their diabetes.
- A – regular A1C tests.
- B – managing blood pressure.
- C – balancing your cholesterol levels.
- S – quit smoking.
Coping with diabetes can also be a challenging journey, with feelings of sadness and anger being common. Practicing meditation, doing a hobby, or talking to your friends or a therapist can help manage stress and depression.
A DIABETES HEALTHCARE TEAM
Diabetes affects different parts of the body, and people who have had the condition for some time might need to see different specialists for specific purposes.
A diabetes healthcare team might include your primary doctor, an endocrinologist (hormone specialist), a dietician, an ophthalmologist (eye specialist), a dentist, a nephrologist (kidney specialist), and a podiatrist (feet doctor) among others.
Treatment for diabetes is patient-centered, meaning that it is tailored around the patient’s needs and complications. Working through the combined efforts of a team significantly reduces the risk of developing serious diabetes complications.
OUTLOOK
Besides diabetes, chronically high blood sugar levels can lead to the development of several complications that affect different parts of your body.
- If you’re in the early stages of diabetes, many of these complications can be prevented through lifestyle interventions.
- However, many acute diabetes complications can happen at any moment and often require immediate medical attention.
Educating yourself about such complications and talking with your doctor about the risk factors are key preventive measures.