The Lamen
Understanding Type 2 Diabetes
Key Takeaways.
Type 2 diabetes is one of the most significant public health concerns, despite the majority of cases being preventable.
Breaking point: The global burden of type 2 diabetes has been increasing steadily, with the International Diabetes Federation predicting over 690 million with diabetes worldwide by 2045.
What's brewing: A class of diabetes drugs has been gaining momentum as potential weight-loss medications, with drugs like Wegovy receiving approval for "chronic weight management in adults with general obesity or overweight."
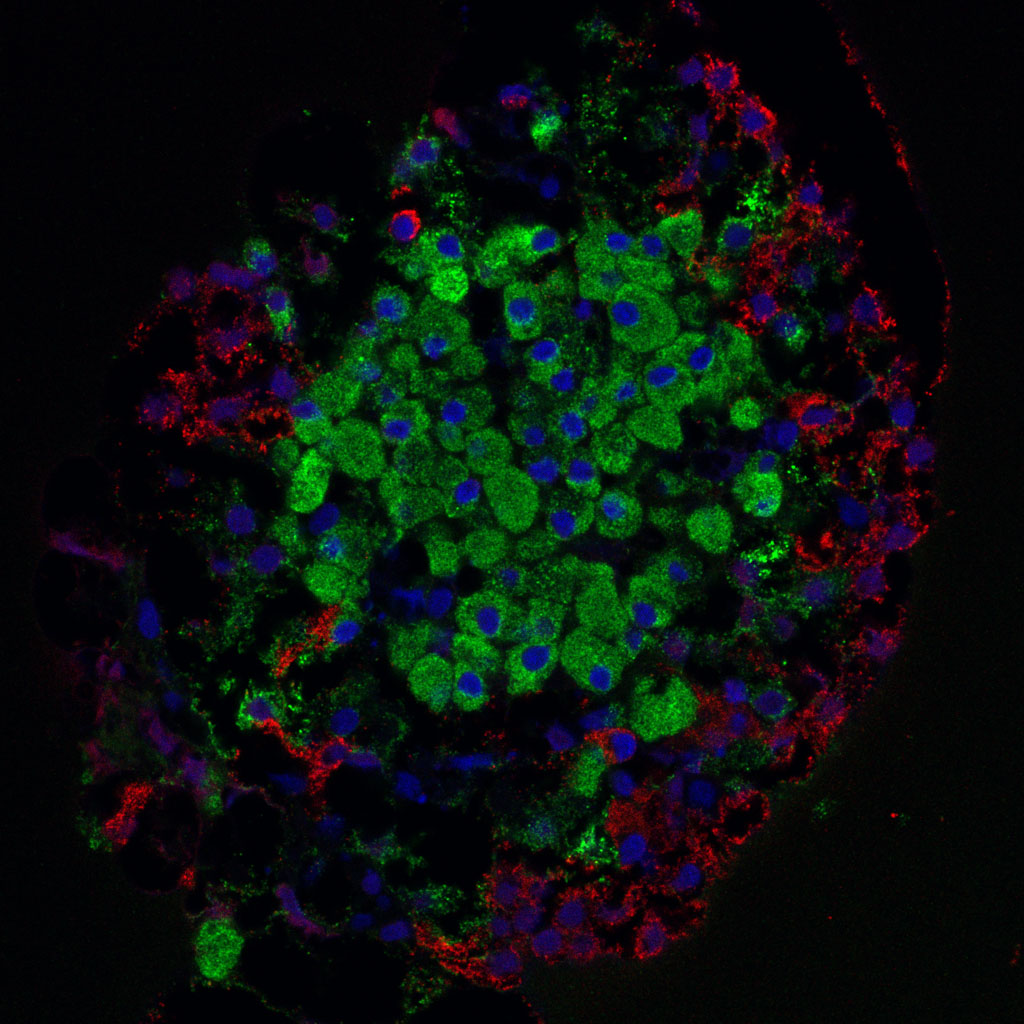
Found in the pancreas, the Islets of Langerhans contain hormone-producing cells, primarily alpha cells (producing glucagon) and β cells (producing insulin). Metabolic and inflammatory cellular stressors eventually result in the death of these β cells, leading to type 2 diabetes.
Image by Creative Commons
Type 2 diabetes is a common chronic metabolic condition that causes persistently high blood sugar, and affects nearly 1 in 10 Americans. It typically occurs when your body doesn’t produce enough insulin – a hormone that converts glucose, or blood sugar, into energy.
Diabetes is broadly classified as type 1 diabetes, type 2 diabetes, and gestational diabetes. Of these, type 2 diabetes accounts for nearly 90 percent of all diabetes cases.
Type 2 diabetes is caused by a combination of genetic and lifestyle factors, and is most often linked to obesity and a sedentary lifestyle.
Uncontrolled type 2 diabetes can lead to the development of several symptoms, some of which can be critical.
What causes type 2 diabetes?
The talk: Despite common belief, it’s not just the overconsumption of sugary foods that causes type 2 diabetes. The condition is actually caused due to impaired insulin secretion and function.
The science: Type 2 diabetes begins with the elevation of blood glucose levels — due to a combination of external and endogenous factors.
- The pancreas makes insulin — the hormone responsible for maintaining blood sugar levels.
- T2D is connected to a condition called insulin resistance, where organs do not respond to insulin effectively, causing the pancreas to overproduce insulin.
- While the pancreas initially works harder to produce more insulin, it loses this ability over time — leading to diabetes.
By the numbers: According to the Centers for Disease Control and Prevention (CDC), nearly 90 percent of U.S. adults diagnosed with diabetes are overweight or obese. Additionally, nearly 35 percent of these people lacked any physical activity throughout the day.
You’re more likely to get diagnosed with type 2 diabetes if:
- you are 45 years or older
- you have a family history of type 2 diabetes
- you are Black, Hispanic/Latino, American Indian, or of Native Alaska descent
Other factors that influence the risk of type 2 diabetes include being prediabetic or having non-alcoholic fatty liver disease.
Early signs and more serious symptoms.
Symptoms of type 2 diabetes tend to develop slowly, typically over several years, beginning with insulin resistance and gradually developing into hyperglycemia. The symptoms are often mild at first and are not noticed until the condition worsens.
The early signs of type 2 diabetes include:
- increased thirst
- frequent urination
- increased hunger
- fatigue
- blurred vision
- slow healing of wounds and sores
- pain, numbness, or tingling sensation in the feet or hands
The milder symptoms of type 2 diabetes are easier to miss. However, as the condition worsens, the symptoms can become more serious and even cause some dangerous complications.
More serious symptoms and complications of high blood sugar levels from type 2 diabetes include:
- heart disease and stroke
- feeling of numbness due to nerve damage (neuropathy)
- eye disease (diabetes-related retinopathy)
- kidney disease (nephropathy)
- gum disease
- skin conditions
- erectile dysfunction
Most people experience type 2 diabetes when they’re adults, although an increasing number of children and teens are developing the condition.
Type 1 vs. Type 2 Diabetes.
The main difference between type 1 and type 2 diabetes is that while type 2 diabetes is primarily influenced by lifestyle factors, type 1 diabetes is a genetic condition typically manifesting early in life.
- Type 1 diabetes accounts for nearly 5 to 10 percent of all diabetes cases, as opposed to the 90 percent of occurrence of type 2 diabetes.
- In the case of type 1 diabetes, your immune system attacks the cells in your pancreas that produce insulin, making your body unable to produce insulin.
- Type 1 diabetes can only be managed by taking insulin externally, while type 2 diabetes can be managed with diet and exercise.
Additionally, type 1 diabetes cannot be prevented, but you can lower your risk of type 2 diabetes through certain lifestyle changes.
Diagnosis.
You should see a doctor if you ever suspect any symptoms of diabetes. Type 2 diabetes is typically diagnosed with a blood or urine test.
Testing for type 2 diabetes may involve the following:
- Hemoglobin A1C test. The A1C test measures your average blood glucose levels over the past 3 months. It does not require you to fast before the test and is reported as a percentage. The higher your percentage, the higher your blood glucose levels are.
- Random plasma glucose test. This test is performed if you have symptoms of diabetes and don’t want to fast for 8 hours before taking the test.
- Oral glucose tolerance test. The doctor takes your blood sample before and after drinking a sugary drink. The test requires you to fast for 8 hours.
- Fasting plasma glucose test. This test measures your blood glucose levels and is done after an 8-hour fast.
During your diagnosis, your doctor will typically ask you about:
- your lifestyle, such as alcohol and smoking
- your diet and physical activity
- whether you have a family history of diabetes
Following through: If you are diagnosed with type 2 diabetes, your doctor will typically follow up with:
- asking you to regularly monitor your blood glucose levels
- making dietary and physical activity recommendations
- prescribing medication, if you need any
- asking you to go for regular type 2 diabetes check-ups
- instructing you to look out for other health problems and complications
Your doctor will typically work with you in deciding your treatment plans, such as the requirement for medication or insulin. You might also visit a dietician or an endocrinologist for specialized diet and insulin management instructions.
Treating type 2 diabetes.
Type 2 diabetes currently has no cure, and the condition is primarily managed through a combination of diet and exercise. The main goal of therapy is to control blood sugar levels, prevent complications, and improve the overall quality of life.
Your healthcare provider will typically ask you to follow a diet low in refined and simple carbohydrates, and high in fiber and healthy fats. Additionally, you will be recommended to perform at least aerobic exercise for 90 to 150 minutes per week.
The therapy is built around the goals of managing your:
- blood sugar
- cholesterol
- blood pressure
Your doctor will monitor your blood sugar levels, and decide on the need for medications based on your condition.
Not everyone with type 2 diabetes needs to take insulin right away. It is typically recommended for people who have had the condition for some time or have significantly higher blood sugar levels.
If you do decide to take insulin, you should always consult your doctor and learn all you can about it before beginning the treatment.
Medications.
If lifestyle changes are not enough to manage type 2 diabetes, your doctor may recommend certain medications that can help with managing your blood sugar levels.
These medications include:
- Metformin. It is typically the first diabetes medication doctors prescribe if lifestyle changes alone aren’t enough for managing your blood sugar levels.
- Sulphonylureas. These work by stimulating the cells in your pancreas to make more insulin and also help insulin work more effectively.
- Dipeptidyl peptidase-4 (DDP-4) inhibitors. These work by blocking the action of DDP-4, an enzyme that destroys the hormone incretin. Incretins help in producing insulin when needed.
- Metglitinides. Taken before each meal, these are fast-action medications that increase insulin production to prevent your blood sugar from increasing.
- Alpha-glucosidase inhibitors. They block the breakdown of starches and some sugars in your intestines, thus helping in lowering blood sugar levels.
- Thiazolidinediones. These work by making your muscle and fat more sensitive to insulin.
- Statins. These are actually blood cholesterol-lowering drugs but are commonly prescribed to people with diabetes as they have an increased risk of heart disease.
Each diabetes medication can have its own side effects, which means that you should talk to your doctor to choose the best medication or combination of medications for your condition.
People with type 2 diabetes usually need insulin only if oral medications and lifestyle changes are not effective in reducing their blood sugar levels.
Insulin is available in different types, including:
- ultra rapid-acting
- rapid-acting (inhaled)
- short-acting
- intermediate-acting
- long-acting
- ultra-long acting
Your doctor will work with you to review your medication options, along with other factors that might influence how much insulin you need. You should follow your doctor’s instructions on when and how to take your insulin.
Living with diabetes.
One of the primary requirements of living with type 2 diabetes is the self-monitoring and management of blood glucose levels. This is done primarily through diet and physical exercise.
• Diet
The diet a person with type 2 diabetes should follow is not fundamentally different that the diet model that most people should follow.
The big difference is that people with diabetes need to stick to their diet, with a single “cheat” being more serious than it would for someone with no such metabolic conditions.
If you’ve been diagnosed with type 2 diabetes, you should avoid processed foods and refined carbohydrates. Additionally, you should avoid any sugary drinks, even fruit juices, as well as fatty or fried foods.
A standard diet for a person with type 2 diabetes should contain foods such as:
- non-starchy vegetables
- whole fruits
- low GI vegetables
- salmon
- sources of healthy fats, such as nuts and avocados
To find out the most optimal diet and portion size for yourself, you can talk to a dietician or spend time researching the foods that are the most helpful in managing blood sugar levels.
• Exercise
The talk: Physical activity is essential in preventing or delaying several chronic conditions, and a similar association has been observed between exercise and type 2 diabetes.
Exercise has both short-term and long-lasting effects on diabetes. In the short term, exercise increases the “fuel use” of your body – which depletes your body of excess glucose.
The evidence: A 2015 study showed that increased physical activity can significantly decrease the risk of developing diabetes, even in very high-risk individuals.
Regular exercise has also been shown to reduce the dependence on oral blood sugar-lowering medications and insulin.
Zooming out: People with type 2 diabetes should aim for at least 30 minutes of moderate to vigorous-intensity workouts, aiming for at least 150 minutes of exercise throughout the week.
These are, however the minimum requirements and more time spent exercising has been associated with better management of the disease.
• Smoking
Everyone knows smoking cigarettes is bad for your health, considering the box itself comes with this warning. However, smoking can lead to the developing and worsening of type 2 diabetes.
The evidence: Nicotine makes it so that your cells don’t respond well to insulin, not to mention the inflammation that inhaling these chemicals causes. According to the CDC, smokers are at a 30 to 40 percent greater risk of developing type 2 diabetes compared to non-smokers.
Alcohol is another tricky subject when associated with type 2 diabetes. While an occasional drink to treat yourself isn’t going to do much harm, overconsumption of alcohol can cause hypoglycemia, obesity, and an increased risk of diabetes.
• Impact on mental health
Besides your metabolic health, diabetes can also lead to changes in mood and even the development of mood disorders.
According to the CDC, people with diabetes are 2 to 3 times more likely to have depression compared to those without diabetes. The occurrence of psychiatric disorders with diabetes is associated with:
- poor quality of life
- increased cost of care
- poor adherence to treatment
- increased risk of diabetic ketoacidosis
- more frequent hospitalizations
People with diabetes may experience delirium, substance abuse, depression, anxiety disorders, schizophrenia, and other psychotic disorders.
If a person notices rapid mood swings or any other symptoms of a mental health condition occurring along with diabetes, they are recommended to see a doctor or a psychiatrist. They should seek immediate medical assistance or call someone they know if having thoughts of self-harm.
Complications.
The longer you’ve had diabetes, the higher your risk for complications. The improper management of blood sugar levels can lead to several health conditions – from your eyes to your feet.
Complications that occur at any time are known as acute complications, and include:
- hypoglycemia, or significantly lower blood sugar levels
- hyperglycemia, or too high blood sugar levels
- diabetic ketoacidosis, which is a life-threatening condition that occurs when your body doesn’t have enough insulin
Type 2 diabetes can also cause conditions that develop over time, known as chronic complications. These include:
- eye problems (retinopathy) can affect eyesight and even cause sight loss
- an increased risk of heart attack and stroke
- diabetics may develop nerve damage (neuropathy) due to high blood sugar levels
- foot problems that may even lead to amputation if left untreated
- skin problems, such as bacterial and fungal infections, and slow healing of wounds and cuts
- kidney disease (nephropathy) which may lead to kidney failure if untreated
- women may experience loss of sensation in sexual organs, sexual dysfunction, and an increased risk of urinary tract infections (UTIs)
- men with type 2 diabetes are 3 times more likely to have erectile dysfunction
While the complications of type 2 diabetes can be serious and even life-threatening in some cases, effectively managing your blood sugar levels can prevent or delay many of these complications.
Are you at risk?
Factors that put you at a greater risk of developing type 2 diabetes include:
- Overweight and obesity. Type 2 diabetes is three to seven times more common in adults with obesity compared to those with normal-weight adults.
- Descent. You are more likely to develop type 2 diabetes if you are African American, Hispanic/Latino, American Indian, or Native Alaskan.
- Family history. You are more likely to get type 2 diabetes if you have a parent, brother, sister, or child with the condition.
- Gender. Type 2 diabetes is slightly more common in men compared to women.
- Smoking is associated with a higher risk of type 2 diabetes.
Besides those mentioned above, people living a sedentary lifestyle or following a diet rich in highly processed foods are at a greater risk of getting type 2 diabetes.
Prevention.
You might not be able to prevent type 2 diabetes in some cases – such as when you’re genetically predisposed to the condition. However, certain lifestyle changes can help you prevent the condition, even if you are prediabetic.
Here are certain tips that can lower your risk of developing type 2 diabetes:
- consuming only unrefined, high-quality carbs
- eating the necessary amount of fiber
- regular aerobic activity
- increasing muscle mass
- quitting smoking
- avoid eating highly-processed foods
According to the CDC, losing 5 to 7 percent of body weight achieved through diet and exercise results in a 58 percent lower incidence of type 2 diabetes, and a 71 percent reduction in people 60 and older.
It is also important to educate yourself about the signs of high blood sugar and prediabetes.
Nearly 80 percent of people with prediabetes don’t know they have it. If you are pre-diabetic, early management of blood sugar levels can significantly reduce the risk of it developing into diabetes.
Statistics for Type 2 Diabetes.
In adults: Here are some statistics for type 2 diabetes in adults reported by the International Diabetes Federation (IDF):
- an estimated 541 million adults are at an increased risk of developing type 2 diabetes in 2021
- 3 in 4 adults with diabetes live in low- and middle-income countries
- Almost 50 percent of adults living with diabetes are undiagnosed
The statistics for diabetes in the U.S. according to the CDC:
- nearly 38 percent of adults (96 million people) have prediabetes
- nearly 48.8 percent of adults 65 years or older have prediabetes
- people with diabetes have nearly 2.3 times greater medical expenses compared to a person without diabetes
In children: Here are the statistics for youth (up to 19 years of age) living with type 2 diabetes:
- 1 in 5 children aged 12-18 years have prediabetes
- prediabetes is more common in males
- type 2 diabetes is the most common in non-Hispanic Blacks or American Indian youth
Additionally, a 2018 study found that the prevalence of type 2 diabetes in youth increases with age.
Researchers believe that the increased prevalence of type 2 diabetes in youth is due to:
- rising rates of childhood obesity
- exposure to maternal obesity and diabetes
- increased diabetes screenings
In different ethnicities: The increased risk of type 2 diabetes in American adults based on their ethnicity:
- American Indians and Alaska Natives: 14.5%
- Non-Hispanic Blacks: 12.1%
- Hispanics: 11.8%
- Non-Hispanic Asians: 9.5%
- Non-Hispanic Whites: 7.4%
Additionally, 13.4 percent of adults with less than a high school education had been diagnosed with diabetes compared to 7.1 percent of those with more than a high school education.
A 2014 study also found that Native Americans, Alaskan Natives, and Hispanic Americans are up to 2.3 times more likely to die from diabetes. Additionally, they are at an increased risk of developing complications.