The Lamen
Breast Cancer Basics: Causes, Types, and Treatment
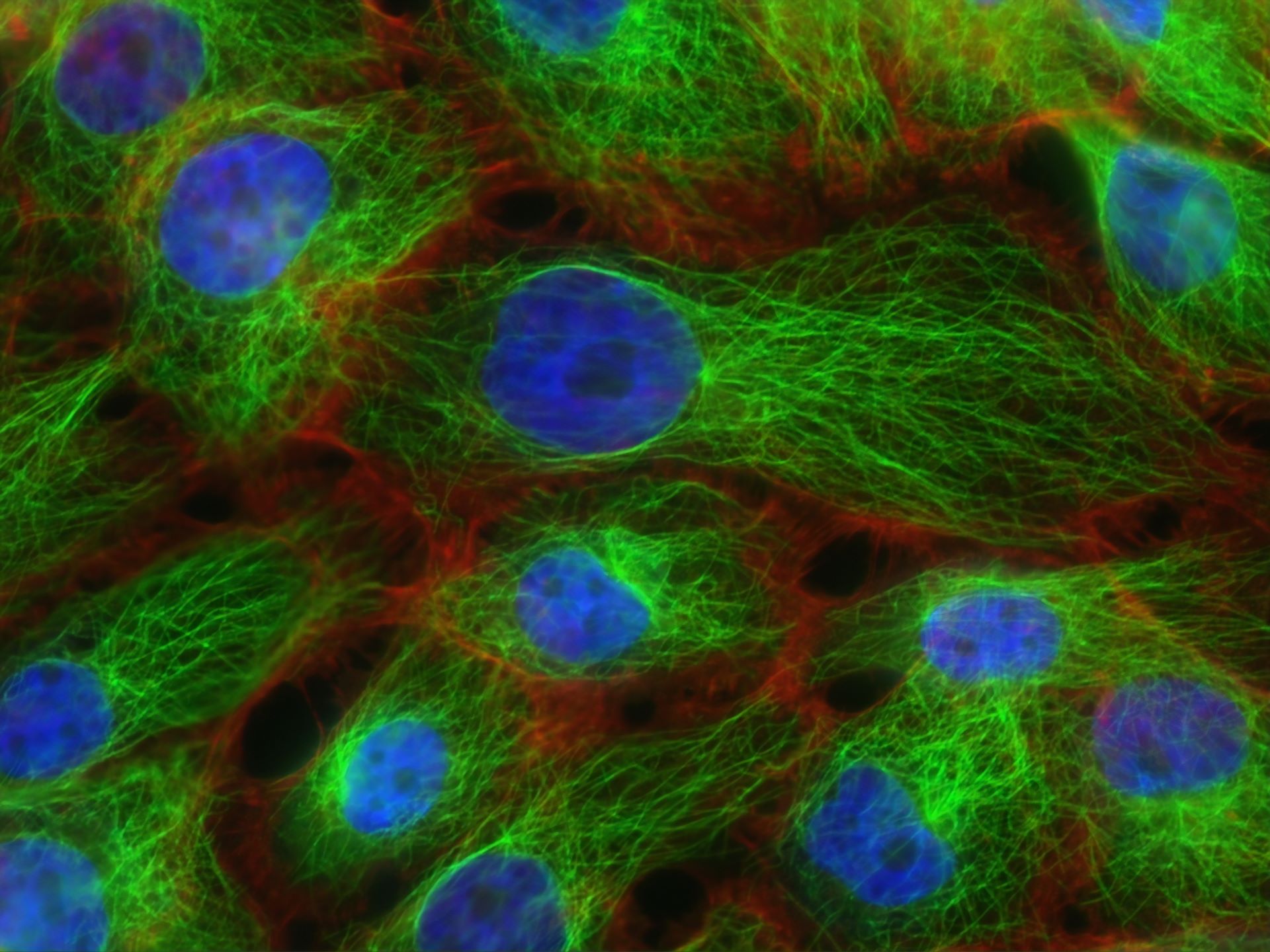
Image acquired with fluorescence microscopy showing stress fibers (red) and microtubules (green) in human breast cancer cells (nuclei, blue). These cytoskeletal proteins are essential for survival and cellular processes in both normal as well as cancer cells. However, these mechanisms can be altered to promote cancer cell growth and invasive capabilities.
Photo: National Cancer Institute
In This Article
Breast cancer is the most common type of cancer (besides skin cancer), with an estimated 300,590 cases expected in the United States in 2023. Unlike common belief, breast cancer can occur in both women and men — caused when cells in the breast mutate and multiply uncontrollably.
What is breast cancer?
Cancer occurs when cells something causes the cells in your body to keep multiplying. This uncontrolled growth can lead to overcrowding of cells, which may form lumps of tissue known as tumors.
When the cancer develops in the breast cells, it’s known as breast cancer. The cancer can form in different areas of the breast, including:
- Cancers that start in the lobules, the glands that produce breast milk, are known as lobular cancers.
- Small canals responsible for carrying the milk to the nipple are known as ducts. Cancers that start here are known as ductal cancers. Breast cancers typically start in the ducts.
- While less common, breast cancers can also begin in the nipple (Paget disease of the breast), breast fat (phyllodes tumor), and blood or lymph vessels (angiosarcoma).
These cancerous cells can spread if they get into the blood or lymph vessels, providing a pathway to other healthy cells of the body. When cancer cells travel and spread to other parts of your body, the cancer is called metastatic.
Early signs and symptoms.
Early detection is key when it comes to treating any type of cancer.
While breast cancer may not cause any symptoms in its early stages, the most common sign is a lump in the breast that was not there before. Not all lumps are cancers, but a hard, painless mass of tissue that has irregular edges is likely to be cancer.
The signs: The symptoms of breast cancer can vary for different people. The most common symptoms of breast cancer include:
- a lump of tissue in your breast that was not there before
- swelling of a part or all of a breast
- breast pain
- nipple pain
- change in size or shape of the breast
- pitted skin on the skin appearing red or discolored (resembling an orange peel)
- inverted nipple
- a discharge from the nipple other than breast milk
- drying, flaking, thickening, or reddening of the nipple or breast
- a lump under the arm
Follow through: While these signs can be warning signs of breast cancer, they can also be caused by a non-cancerous condition like a cyst.
If you experience any of the symptoms above, you need to see a doctor who will conduct the appropriate tests to check whether you have breast cancer.
Types of breast cancer.
There are several types of breast cancer, which are typically categorized by where the cancer originates in the breast.
In general, breast cancers are broken down into 2 main categories:
- in situ or non-invasive cancer
- invasive cancer
An invasive cancer is one that has spread into the surrounding breast tissue, whereas non-invasive cancer has not spread beyond the site of origin.
• Ductal carcinoma in situ (DCIS)
Ductal carcinoma in situ (DCIS) is a noninvasive cancer accounting for nearly 1 in 5 new breast cancer cases.
With DCIS, the breast cancer is confined to the walls of the ducts and has not spread to nearby breast tissue. Nearly all women detected at this early stage can be cured of breast cancer with effective treatment.
However, DCIS can sometimes become invasive if left untreated.
• Lobular carcinoma in situ (LCIS)
Lobular carcinoma in situ (LCIS) refers to cells growing in the lining of milk-producing glands called lobules. Like DCIS, the cancerous cells in lobular carcinoma in situ haven’t invaded the nearby breast tissue.
The types of LCIS include:
- classic LCIS
- pleomorphic LCIS
- florid LCIS
While LCIS does not spread beyond the lobule even if it isn’t treated, it does run the risk of developing into invasive breast cancer.
• Invasive ductal carcinoma
Invasive ductal carcinoma starts in the milk duct in the breast but can spread into nearby tissues by breaking through the duct wall.
According to the American Cancer Society, about 8 in 10 invasive breast cancers are invasive ductal carcinomas — making it the most common type of breast cancer.
• Triple-negative breast cancer
Triple-negative breast cancer refers to cancers satisfying specific conditions and accounts for nearly 10 to 15 percent of all breast cancers, according to the American Cancer Society.
To be diagnosed with triple-negative breast cancer, a tumor must:
- Lack estrogen receptors.
- Lack progesterone receptors.
- And not make too much or any of the protein called HER2.
Because triple-negative breast cancers lack the estrogen and progesterone receptors and don’t make too much of the HER2 protein, they don’t respond to hormonal therapy.
Triple-negative breast cancers tend to grow and spread more quickly and are more likely to return after treatment compared to other types of breast cancer.
• Inflammatory breast cancer
Inflammatory breast cancer (IBC) is a rare but aggressive type of breast cancer – accounting for only 1 to 5 percent of all breast cancer but almost always detected at an advanced stage.
Inflammatory breast cancer is a type of invasive ductal carcinoma but with different symptoms and treatments. It occurs when cancer cells block the lymph vessels in the breast, causing the breast to look red, swollen, and feel warmer and heavier.
The survival rates for inflammatory breast cancer are not as high as other types of breast cancer, particularly because IBC has already metastasized by the time of diagnosis in about 1 in 3 cases.
• Angiosarcoma
Angiosarcoma is cancer that starts in the cells lining the blood or lymph vessels in the breast and accounts for less than 1 percent of all breast cancers.
The condition can cause skin changes in the breast, leading to the appearance of purple-colored nodules.
Breast cancer in men.
The most common types of breast cancer are the same for both men and women, and the symptoms that they experience are typically identical.
A healthier lifestyle, including a healthy weight and limiting alcohol consumption, seems to lower the risk of developing breast cancer in both women and men.
By the numbers: Male breast cancer is rare, accounting for nearly 1 percent of all breast cancer cases diagnosed in the U.S. However, breast cancer is often diagnosed late in men, leading to lower survival rates, ranging from 40 to 65 percent.
The ACS reports that the risk of breast cancer is about 70 times less among Black men compared to Black women. This risk is about 100 times lower in White men compared to White women.
The Stages.
The process of staging breast cancer involves determining if the cancer has spread and to what extent.
According to the ACS, the following factors are considered when staging breast cancer:
- size of the tumor (T)
- if the tumor has spread to nearby lymph nodes (N)
- if the tumor has metastasized (M)
- status of estrogen receptor (ER)
- status of progesterone receptor (PR)
- grade of cancer (G)
- HER2 protein status
Based on these, breast cancer is given one of five main stages.
• Stage 0
The cancer is in situ, that is, the cells remain confined in their site of origin and have not spread to any nearby tissue.
• Stage 1
- Stage 1A. The cancer is 2 cm or smaller and has not spread outside the breast.
- Stage 1B. The cancer cells are found in lymph nodes closest to the breast. If a tumor is found, it is smaller than 2 cm.
The breast cancer is small and is confined only to the breast tissue, or in the lymph nodes close to the breast.
• Stage 2
Stage 2A.
- There is either no tumor or a tumor 2 cm or smaller and the cancer cells are found in 1 to 3 lymph nodes, or the tumor is between 2 to 5 cm but is not found in the lymph nodes.
Stage 2B.
- the tumor is between 2 and 5 cm with small areas of cancer cells in the lymph nodes;
- the tumor is between 2 and 5 cm and the cancer has spread to 1 to 3 lymph nodes;
- or the tumor is larger than 5 cm but hasn’t spread to the lymph nodes.
The breast cancer is either in the breast, in the nearby lymph nodes, or both.
• Stage 3
Stage 3A.
- no tumor found in the breast or the tumor may be of any size, found in 4 to 9 lymph glands;
- the tumor is larger than 5 cm with small clusters of cancer cells in the lymph nodes;
- the tumor is larger than 5 cm and has spread into up to 3 lymph nodes.
Stage 3B.
- The tumor has spread to the skin of the breast or the chest wall, and may or may not have invaded up to 9 lymph nodes in the armpit.
Stage 3C.
- There may be no tumor, or it may be of any size. However, the cancer cells have spread to the skin of the breast, causing swelling or an ulcer.
- It may also have spread to 10 or more lymph nodes in the armpit, lymph nodes near the breastbone, or internal mammary nodes.
The cancer has spread from the breast to lymph nodes close to the breast or to the skin of the breast.
• Stage 4
The breast cancer has metastasized — meaning that the cancer has spread to other parts of the body. It is also known as advanced or metastatic breast cancer.
Diagnosis.
If you experience a lump in your breast or any other symptom of breast cancer, your doctor will typically conduct a physical breast exam along with screening tests to determine your condition.
A breast cancer diagnosis can include the following tests:
- Mammogram. A mammogram is a low-dose X-ray that can often show any abnormalities in the breast, including calcifications, masses, distortions, and asymmetries. It is the most common screening test for breast cancer. The American Cancer Society recommends that women between 45 and 54 should get mammograms every year.
- Breast ultrasound. This uses sound waves to create computer-generated images of the inside of the breast. It involves putting a gel on the skin of the breast and then moving a device called the transducer over the skin. Ultrasounds are able to detect and tell the difference between fluid-filled masses like cysts and solid masses.
- Breast MRI. A breast MRI (magnetic resonance imaging) utilizes radio waves and strong magnets to create detailed pictures of the inside of the breast. A breast MRI is recommended along with a yearly mammogram for women who are at a high risk for breast cancer.
- Biopsy. A biopsy is typically done if a mammogram (or other imaging tests) shows a change in the breast that could be cancer. It involves removing small pieces of breast tissue and examining them in the lab to see if they are cancerous.
A biopsy is the only way to know for sure if you have breast cancer. If the sample tests positive for cancer, your doctor will recommend the next steps in treatment.
Treatment.
Treatment for breast cancer depends on a variety of factors, including:
- location of the tumor
- size of the tumor
- stage and grade of the tumor
- age of the patient
Surgery is the most common treatment for breast cancer and is often a part of treatment to remove as much of the cancer as possible. Other treatment options include chemotherapy, hormone therapy, and radiation therapy.
• Surgery
Breast cancer surgery is performed to remove as much of the cancerous tissue from the breast as possible.
There are multiple types of surgery for breast cancer depending upon the conditions, including:
- Lumpectomy. This removes the tumor along with a small portion of the healthy tissue surrounding it.
- Mastectomy. A mastectomy involves the removal of the entire breast. In some cases, a doctor may perform a nipple-sparing mastectomy to retain the nipple and areola. It can be followed up by breast reconstruction.
- Sentinel node biopsy. It involves the removal of the lymph nodes that have been invaded by cancer cells. If a tumor is not detected in the first lymph node that cancer would spread to, others don’t need to be removed.
- Axillary lymph node dissection. If multiple lymph nodes are detected with cancer cells during the sentinel node biopsy, the doctor may remove additional lymph nodes.
While surgery is effective in curing localized breast cancer, it is unlikely to cure cancer that has spread to other parts of the body.
• Radiation therapy
Radiation therapy uses high-energy radiation to destroy cancer cells. The process is often conducted after surgery when treating the early stages of breast cancer.
There are two main types of radiation therapy used to treat breast cancer:
- External beam radiation therapy. This is the most common type of radiation therapy used for women with breast cancer. It involves the use of a large machine called the linear accelerator outside the body to focus radiation on the cancer cells.
- Brachytherapy. Also known as internal radiation, brachytherapy involves placing a device containing radioactive pellets into the breast tissue for a short duration. This aims at the cancer cells from inside the body.
Radiation therapy for breast cancer is typically performed after a lumpectomy or mastectomy to remove any cancer cells that may have been left behind during the surgery.
• Chemotherapy
Chemotherapy uses anti-cancer drugs such as anthracyclines and taxanes that may be given intravenously or orally. It is typically used in conjunction with other forms of treatment, typically surgery.
- It may be performed before surgery in an attempt to shrink the tumor to avoid extensive surgery. In other cases, chemotherapy is used after lumpectomy or mastectomy to kill any cancer cells that may have been left behind.
Side effects: Chemo can also lead to a number of side effects, the most common of which include:
- hair loss
- mouth sores
- loss of weight
- diarrhea
- fatigue
- menstrual changes
- nerve damage
While these side effects typically go away after the treatment is finished, you should discuss any concerns with your doctor if you are considering the treatment.
• Hormone therapy
Some breast cancers are affected by hormones such as estrogen and progesterone. According to the American Cancer Society, 2 out of 3 breast cancer are hormone-receptor positive — meaning that they need a certain hormone to grow.
- Estrogen and progesterone — commonly identified as female hormones — help breast cancer tumors grow. Hormone therapy blocks the production of these hormones in the body or blocks the hormone receptors on the cancer cells.
- It involves the use of drugs such as selective estrogen receptor modulators (SERMs), aromatase inhibitors (AIs), and selective estrogen receptor degraders (SERDs).
Hormone therapy may help slow down or stop the growth of the tumor. The treatment is typically performed for at least 5 years.
• Immunotherapy
Immunotherapy boosts your body’s own immune system to fight off cancer cells more effectively. It does so with the use of immunotherapy drugs such as monoclonal antibodies checkpoint inhibitors.
• Other medications
Cancer cells can also be specifically destroyed by targeted drug therapy, which involves the use of medications that attack mutations within cancer cells.
Some of the most common drugs used to treat breast cancer include:
- trastuzumab
- pertuzumab
- emtansine
- lapatinib
You should talk to your doctor about the potential side effects of any of these medications before deciding on the appropriate treatment.
The risk factors.
- Being overweight or obese. Having more fat after menopause can raise estrogen levels, increasing the risk of developing breast cancer. Postmenopausal women are 1.4 to 2 times more likely to develop breast cancer if they are obese or overweight.
- Alcohol and smoking. Compared to women who don’t drink, those who have 3 alcoholic drinks per week have a 15 percent higher risk of breast cancer — which goes up by 10 percent for each additional drink. Even moderate alcohol consumption has been linked to a 30 to 50 percent increase in breast cancer.
- Physical inactivity. Studies have shown that physically active women have a 16 to 21 percent lower risk of developing breast cancer.
- Getting older is something you cannot prevent, and your risk of developing breast cancer goes up as you age. Most breast cancers are diagnosed after the age of 50.
- Breast implants. While breast implants have not been linked with an increased risk of common types of breast cancer, the ACS reports that it has been linked with lymphomas.
- Having dense breast tissue. Women with denser breasts have more glandular and fibrous tissue, and less fatty tissue — and a greater risk of breast cancer. Breast density can be influenced by factors such as age, genetics, pregnancy, and certain drugs.
- Hormone therapy. People who take postmenopausal estrogen and progesterone to relieve the symptoms of menopause may be at an increased risk of breast cancer.
- Genetic factors. While being born female already puts you at a greater risk of breast cancer, the condition can also be influenced by genetic factors. In fact, 5 to 10 percent of all breast cancer cases are considered hereditary.
Besides those stated above, other factors that could increase the risk of breast cancer include not having children, not breastfeeding, certain birth control drugs, and diet.
Breast cancer in different ethnicities.
The ACS reports that white women are at a slightly higher risk of developing breast cancer compared to African American women. However, the difference has been reducing in recent years.

Female breast cancer incidence (2015–2019) and mortality (2016–2020) rates by race/ethnicity in the United States. Data: American Cancer Society Journals
Graph by The Lamen
- Non-Hispanic white: 1 in 100,000
- Hispanic or Latina: 91 in 100,000
- African American: 3 in 100,000
- Asian American: 3 in 100,000
- American Indian or Alaska Native: 1 in 100,000
Studies have also shown that race, ethnicity, and socioeconomic status are integral in determining the detection and effective treatment of breast cancer.
Breast cancer survival rates.
Survival rates of cancers are estimates, and the survival rate of breast cancer depends on a variety of factors.
These factors include:
- age
- race and ethnicity
- gender
- type of breast cancer
- growth rate
- lifestyle factors
By the numbers: The 5-year survival rate for women in the United States with non-metastatic invasive breast cancer is 91 percent. The survival rate decreases to 85 percent at the 10-year mark.
- However, the survival rates for breast cancer can vary significantly with the region. The breast cancer survival rate is approximately 80 percent in North America, 60 percent in Japan and Sweden, and less than 40 percent in low-income underdeveloped countries.
Additionally, the mortality rate for Black women (28.4 per 100,000 women) is significantly higher than that of White, Hispanic, and Asian women.
More Statistics.
Here are some statistics for breast cancer from the American Cancer Society:
- Breast cancer accounts for 30 percent of all new female cancers each year.
- Breast cancer in men accounts for less than 1 percent of all breast cancer cases.
- The incidence of breast cancer has increased by half a percent per year in recent years.
- An estimated 43,700 women will die from breast cancer in 2023 – being the second leading cause of cancer death in women.
- Men are more likely to be diagnosed at an advanced stage.
- Black women have a higher chance of developing breast cancer before the age of 40 compared to white women.
- Black women have the highest death rate from breast cancer.
- 1 in 8 women in the United States will develop breast cancer sometime in their life.
Living with breast cancer.
Breast cancer is often a life-changing event, and one cannot anticipate the condition under normal circumstances. If you’ve been diagnosed with breast cancer, you may feel upset, shocked, and frightened.
While many women can get treated when breast cancer is detected early, they might worry about it coming back or even affecting their lifestyle.
Even if you have completed your breast cancer treatment, you will typically still require follow-up checkups involving physical exams and mammograms.
To cope with the changes in life during this period, you should:
- educate yourself about the condition
- talk to other people who underwent breast cancer treatment
- improve your lifestyle
- talk to your partner about your sex life
With coping techniques and treatment, even women who have been detected with an advanced breast cancer may continue to live for several years.
Can you prevent breast cancer?
Cancer is caused when cells grow uncontrollably, often due to mutations that inactivate the genes that suppress cell proliferation. As such, some risk factors such as genetics cannot be avoided, certain lifestyle changes have been shown to decrease the risk of developing breast cancer.
- A healthier lifestyle. Obese or overweight women are at a higher risk of developing breast cancer – especially after menopause. Eating a healthy diet and getting regular exercise is essential in managing your weight and lowering your risk of breast cancer.
- Regular screening. The United States Preventive Services Task Force (USPSTF) recommends that women who are between 50 and 74 years and at average risk of breast cancer should get a mammogram every 2 years. They may even choose to start receiving regular screening earlier.
- Genetic counseling. If you believe that you might have inherited the gene that increases breast cancer risk (BRAC1 or BRAC2 gene), you can receive genetic counseling for breast cancer or use a service such as 23andMe.
- Medications. The ACS recommends that women at an increased risk of breast cancer should take prescription medications that lower breast cancer risk and may even undergo preventive surgery.
While these factors may reduce the probability, they do not ensure that you will not develop cancer. However, they can help with increasing the chances of successful treatment and survival.