The Lamen
Skin Cancer: Everything You Need To Know
Key Takeaways.
Skin cancer may initially appear as something new, changing, or not healing on your skin.
The talk: The most common type of cancer, skin cancer often develops in hard-to-find locations which makes their identification even harder. However, regular screenings and early detection make the majority of cases treatable.
What's brewing: Researchers have been working on a new artificial intelligence pipeline that uses deep convolutional neural networks (DCNNs) to analyze suspicious pigmented lesions (SPLs), which can be an indication of skin cancer — all through your smartphone's camera.
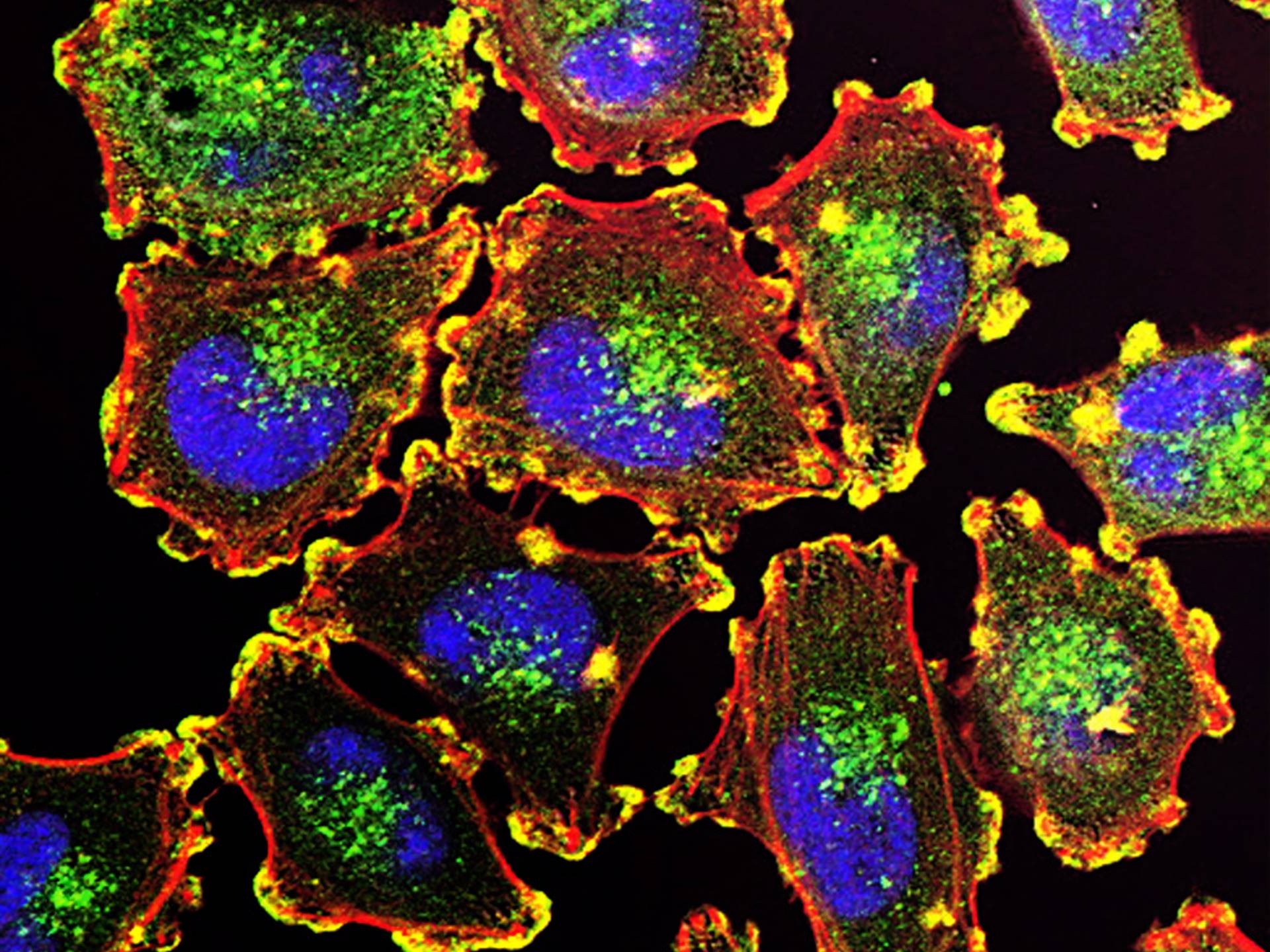
Melanoma cells are highly angiogenic, meaning is highly capable of forming blood vessels needed for the tumor to grow. Additionally, melanoma cells that pass through the before entering the bloodstream spread and form new tumors more readily than cells that directly enter the bloodstream.
Image by the National Cancer Institute/Unsplash
Skin cancer occurs when irregular growth of skin cells occurs. Caused by damage to the DNA, these mutated skin cells multiply rapidly to form tumors. Dermatologists study these cells to identify the type of skin cancer.
There are three major types of skin cancer – basal cell carcinoma, squamous cell carcinoma, and melanoma. Identifying each type gives you the best chance at early detection of skin cancer, providing you with chances of more successful treatment.
Most common skin cancers.
Skin cancer can appear in a number of shapes, sizes, and forms. The most common types of skin cancer are basal cell carcinomas (BCC), squamous cell carcinomas (SCC), and melanomas, while actinic keratosis is the most common precancerous condition.
• Basal cell carcinoma
The talk: Basal cell carcinoma is the most common type of skin cancer. It begins in the basal cells, found at the bottom of the epidermis – the outermost layer of the skin. Basal cells are the ones that produce new skin cells.

Basal cell carcinoma (BCC) accounts for nearly 90 percent of skin cancer cases in the U.S., and develops primarily due to exposure to UV light. However, about 20 percent of BCC cases arise without sun-exposure. It typically presents itself as a shiny, pink, or flesh-colored papule or nodule, which may form into an ulcer over time.
Image by the National Cancer Institute
What to look for: Basal cell carcinomas most commonly develop in areas exposed to the sun, especially the face, scalp, neck, and shoulders. These are caused by the combination of intense short-term exposure and cumulative long-term exposure to UV radiation from the Sun.
In most cases, basal cell carcinoma does not spread to other areas of the body. In rare occurrences, however, these can be life-threatening.
• Squamous cell carcinoma
Squamous cell carcinoma arises from the squamous cells of the epidermis. These are the cells located near the surface of the skin, appearing like fish scales.
Squamous cells are also found in the lining of hollow organs, the lungs, and mucous membranes. These cells can also turn cancerous. To differentiate the two, squamous cell carcinoma of the skin is called cutaneous squamous cell carcinoma.
Cumulative, long-term exposure to the sun’s UV radiation is the most common cause of this type of cancer. They are most common in areas of constant sun exposure, like the face, neck, or head.

Caused due to the uninhibited, accelerated growth of squamous cells, squamous cell carcinoma (SCC) typically appear as scaly red patches, raised growths with a central depression, or open sores.
Image by the National Cancer Institute
By the numbers: According to the American Cancer Society, squamous cell carcinomas are the second most common type of skin cancer (in the US), with about 3.3 million annual cases.
While untreated squamous cell carcinomas can grow into deeper layers of the skin and spread to other parts of the body, they are usually easily treated. Nearly 15,000 deaths occur due to this cancer each year in the U.S.
• Melanoma
Melanomas (also called malignant or cutaneous melanoma) are often confused with moles, and may even arise from them.
What to look for: Melanomas can appear in any area of your body but are more likely to start on the chest and back for men and on the legs in women.
This type of cancer begins in cells known as melanocytes, which give your skin its color. Noncancerous moles are formed by melanocytes.

Melanoma often occurs in hard-to-spot places on the body, and may be pinkish, reddish, white, or even clear, making them hard to recognize. Melanomas are typically characterized as dark spots that stand out from your other moles.
Image by the National Cancer Institute
- It is more than 20 times more common to occur in whites than in African Americans. The lifetime risk of developing melanoma is about 1 in 38 for whites.
- The risk of melanoma also increases as people age.
- About 7,650 deaths due to melanoma are expected to occur in the United States in 2022.
Melanomas are treatable when detected early. However, they can metastasize (spread) without treatment, becoming more complicated. This type of cancer is also more likely to spread to other parts of the body compared to basal and squamous cell cancers.
• Actinic keratosis
Actinic keratosis is the most common precancer (a condition associated with an increased risk of developing into cancer), caused by skin damage by chronic exposure to ultraviolet rays. An estimated 58 million Americans have one or more actinic keratoses.
These often appear as small dry, scaly, or crusty patches of lesions on sun-exposed areas like the face, scalp, forearms, and neck.
If left untreated, these can develop into squamous cell carcinomas.
Rarer skin cancer types.
• Merkel cell skin cancer
Merkel cell cancer is a rare, aggressive form of cancer with about 3,000 cases diagnosed in the U.S. annually.
Its incidence has been steadily increasing and is expected to keep doing so. It is caused by the overgrowth of Merkel cells – a specialized cell found right below the epidermis and often termed “touch receptors.”
What to look for: Merkel cell cancer is usually found in the head and neck region, being especially common in elderly white males. They often appear as firm, painless lesions on a sun-exposed area, resembling pimples.
These grow rapidly and have a high risk of recurring and spreading to other body parts.
• Lymphoma
Lymphoma is a type of cancer that starts in white blood cells called lymphocytes. These cells are part of the immune system’s defense against diseases and infections. Lymphomas are of two main types:
- Hodgkin lymphoma
- Non-Hodgkin lymphoma (Includes all skin lymphomas)
When a non-Hodgkin lymphoma starts only in the skin, it is called a skin lymphoma or cutaneous lymphoma.
Scientists don’t clearly understand the causes of skin lymphoma. It is suggested that certain DNA mutations might cause such cancers. They also believe that people with weakened immune systems have a greater chance of developing skin lymphoma.
According to the American Cancer Society, there were nearly 80,500 new cases of skin lymphoma in the U.S. in 2022, with an estimated 20,250 deaths.
• Kaposi sarcoma
Kaposi sarcoma is a cancer that develops from the cells lining lymph or blood vessels, often appearing as tumors on the skin. These tumors look like purple, red, or brown patches on the skin.
The skin lesions of Kaposi sarcoma most often appear on the legs or face, which may sometimes cause the legs or feet to swell painfully.
Kaposi sarcoma is of four different types:
- Epidemic (AIDS-associated)
- Classic (Mediterranean)
- Endemic (African)
- Iatrogenic (Transplant-related)
These usually don’t show any symptoms. However, if the lesions are formed in the lungs, liver, or digestive tract, they can cause serious internal bleeding and even death.
• Dermatofibrosarcoma protuberans (DFSP)
DFSP is a rare skin cancer that begins in the dermis – the middle layer of the skin. They first appear as a small patch on the skin, looking like a pimple or a rough patch of skin.
Dermatologists found that black people were more likely to get DFSP compared to whites, although they don’t yet know of a definitive cause.
DFSP has a low instance of spreading and a high survival rate, but timely treatment is crucial. If left unattended, these can grow into fat, muscle, or even bone.
• Sebaceous carcinoma
Sebaceous carcinoma is an aggressive skin cancer that develops in the sebaceous gland. The gland is found on most areas of our skin, producing sebum to keep the skin moisturized.
Sebaceous carcinoma tends to develop in and around the eyes, as the area has the greatest concentration of sebaceous glands.
While most growths do not spread, there have been cases of deaths caused due to its metastasizing. Therefore, immediate diagnosis and treatment should be sought.
Symptoms.
The most common signs of skin cancer include:
- Asymmetry: If the two halves or a mole or lesion are not identical.
- Growth and Altering: If you notice any changes in a mole, like size, shape, color, or experience itching or bleeding.
- Skin lesions: A scaly patch, a new mole, a dark spot, or unusual growths, bumps, and scars that don’t disappear.
- Color: Any spot that appears distinctly different from your skin color, like red, white, pink, black, brown, or blue.
- Size: Any patch or mole larger than about one-fourth of an inch can be a warning sign. Most melanomas are larger than 6mm (1/4 inch) in diameter.
Skin cancers come in various appearances, many of which might not be identifiable or even visible. Any unusual change in your skin can be a sign of caution, and you should seek an immediate medical diagnosis in such cases.
• Basal cell carcinoma: Warning signs
Checking areas most commonly exposed to the sun is most important when checking for basal cell carcinomas. However, they may also occasionally develop in other places.
According to the Skin Cancer Foundation, two or more of the following symptoms appear as a sign of a BCC tumor:
- an open sore that doesn’t heal; may bleed, ooze or crust, or return sometime after healing
- a small pink growth with slightly raised edges and an indent in the center, which may sometimes grow atypical blood vessels
- a reddish pat that itches, crusts, or hurts
- a shiny bump that may be clear, pink, red, or white, sometimes tan or brown in people of color
- a pale or yellow-looking scar-like area
Basal cell carcinomas are the most common type of skin cancer.
• Squamous cell carcinoma: Warning signs
A squamous cell carcinoma can take various appearances according to the ADD, and could look like any of the following:
- a rough or reddish scaly patch
- an open sore with or without raised borders
- a firm, dome-shaped growth
- a sore developing in an old scar
- wart-like growth
- a brown spot that resembles an age spot
Squamous cell carcinomas usually appear on the skin with cumulative, long-term sun exposure, like the face, scalp, ears, or neck. It can also be a result of indoor tanning.
• Melanoma: Warning signs
The easiest way to recognize the warning signs of melanoma is through the “ABCDE” signs:
- Asymmetry: Most melanomas are asymmetrical, with the two halves of a lesion or mole not matching.
- Border: They tend to have an uneven border (unlike most moles) with notched edges.
- Color: Melanomas may have multiple shades of brown, tan, or black, and may change in appearance as it grows.
- Diameter or Dark: Melanomas are most commonly larger than 6 mm, or ¼ inch, and often appear darker than other moles or lesions.
- Evolving: Any change in size, shape, color, or new symptoms like bleeding, crusting, or itching could be a sign of melanoma.
Any unusual or rapid changes in a mole or lesion on your skin could be a sign of melanoma, and you should seek a dermatologist immediately.
Stages of skin cancer.
The stage refers to the extent of severity of cancer, and it depends upon the following factors:
- (T – Tumor) size of the tumor
- (N – Node) if the tumor has spread to the lymph nodes; if yes, where, and how many?
- (M – Metastasis) if the tumor has metastasized (spread)
For cancer staging, skin cancers are divided into two main groups: non-melanoma skin cancer and melanoma.
Stages of non-melanoma skin cancers.
- Stage 0: Also called carcinoma in situ. This means that while cells have started to turn into cancer, they have not yet grown or spread beyond the epidermis.
- Stage 1: The cancer may have spread to the next layer of skin, but is 2 centimeters or smaller.
- Stage 2: This means that the tumor is larger than 2 centimeters across, but has not spread to the lymph nodes or nearby sites.
- Stage 3: It means that cancer has not spread to any lymph nodes, but has grown into nearby bones or the subcutaneous tissue (fat under the skin), and is larger than 3 centimeters.
- Stage 4: The cancer has spread beyond the primary tumor site to the lymph nodes. It could also be of any size larger than 3 centimeters and could have spread to distant parts like the lungs.
Melanoma is most often staged by the American Joint Committee on Cancer (AJCC) TNM system, based on tumor, nodes, and metastasis. Once a person’s T, N, and M categories have been determined; the information is combined in a process called stage grouping to assign an overall stage.
The cancer is usually staged using the pathological or surgical stage. However, if surgery is not possible, the cancer is given a clinical stage, based on the results of physical exams, biopsies, and imaging methods.
Stages of melanoma.
- Stage 0: The cancer is still confined to the outermost layer of the skin, the epidermis. Also known as melanoma in situ.
- Stage 1: The tumor has not spread to nearby lymph nodes or any distant parts of the body, but may have spread to the skin’s second layer – the dermis. It is no more than 2 millimeters across.
- Stage 2: The cancer has not spread beyond the original tumor site but could be thicker and larger, but no more than 4 millimeters. It may also show signs like scaling, flaking, or bleeding.
- Stage 3: The cancer has spread to your lymph nodes or to nearby skin or tissue. This stage is divided into 4 sub-stages – 3A, 3B, 3C, and 3D.
- Stage 4: This is the most advanced stage, with the cancer having grown in size and spread beyond the original tumor site. It can show up in the lymph nodes, organs, or distant body parts.
Although each person’s cancer experience is unique, cancers at similar stages tend to have a similar treatment method.
What causes skin cancer?
The talk: The exact cause of cancer remains unclear. Researchers believe there is no single cause for cancer. The interaction of many factors leads to cancer, which could be genetic, environmental, or behavioral.
Current perspectives: Like other types of cancer, skin cancer is caused due to DNA damage and genetic mutations in your skin cells. The mutated cells grow uncontrollably, forming a mass of cancer cells known as a tumor.
• The Sun and UV rays
Most skin cancers are a result of overexposure to UV rays in sunlight. It can be observed that basal and squamous cell carcinomas tend to occur on sun-exposed parts of the body.
The most common sources of UV light are:
- the sun
- tanning beds
- sun lamps
- black-light lamps
- plasma torches and welding arcs
UV radiation is divided into 3 main groups: UVA rays, UVB rays, and UVC rays. Of these, UVB rays are the most associated with skin cancers, although each type can play a role in developing it.
The extent of damage from UV exposure depends on multiple factors, like the strength of the rays or the duration of exposure. It is, therefore, key to protecting yourself from these damaging rays.
• Family history
What to know: Skin cancer can run in families. According to the Skin Cancer Foundation, about 10 percent of patients diagnosed with melanoma have a family history of the disease. If one or more close biological relatives of yours had melanoma, you are at an increased risk.
A family history of basal cell carcinoma is also associated with an increased risk of early onset. According to a study, the sharing of certain lifestyle factors among close relatives might be the reason behind this association.
Following through: If you have a family history of skin cancer, you should take the following steps:
- Protect against UV rays. Protection from UV radiation is still the simplest yet most effective way of reducing your risk of skin cancer.
- More frequent inspections. Be on the lookout for any unusual changes in your skin and moles, self-checking once every month.
- Start early. A familial history of skin cancer increases your risk of early-onset skin cancer. Therefore, you should start being vigilant about your skin starting at puberty.
Regular visits to your dermatologist or talking with someone in your family who experienced skin cancer can also help you.
• Many moles
Moles don’t always indicate skin cancer, but people with multiple of these small brown marks are at an increased risk of developing melanoma.
Most melanomas develop in normal skin, and only about 20 to 30 percent of melanomas arise from pre-existing moles. Atypical moles and many moles put you at an increased risk, and require you to regularly inspect new or changing moles.
• Lighter skin and hair color
Although anyone can get skin cancer, even if they do not easily get sunburned, people with fairer skin have a higher risk.
People with lighter-colored skin, especially with blond or red hair, blue eyes, and freckles are at an increased risk of developing melanoma. Additionally, people who get easily sunburned rather than getting tanned are at a higher risk.
• Weakened immune system
If your immune system is weakened as a result of medical treatments like chemotherapy, an organ transplant, or if you have a medical condition like HIV, you are at a higher risk of developing skin cancer.
• Previously had skin cancer
If you’ve had skin cancer before, you are at a higher risk of the cancer reoccurring. This risk is associated with melanomas, basal cell, and squamous cell carcinomas.
Between 30 to 50 percent of people with non-melanoma skin cancer develop a second non-melanoma skin cancer within 5 years. Regular follow-ups and self-examinations are key for preventing and catching second skin cancers.
In people of color.
People of all colors can get skin cancer. Even if you never get sunburns, you are not completely safe from skin cancer.
Here are some stats for cancer in people of color:
- skin cancer represents 1 to 2 percent of all cancers in Black people
- squamous cell carcinoma is the most common skin cancer in Black people
- Black patients are more than three times as likely to be diagnosed with melanoma at a late stage compared to non-Hispanic white patients
- it represents 4 to 5 percent of all cancers in Hispanic people
- Basal cell carcinoma is the most common in Hispanics
- it represents 2 to 4 percent of all cancers in Asian people
- incidence of non-melanoma skin cancers has been increasing by 3 to 8 percent annually in Asian people
Dark skin has larger melanocytes, producing more melanin. This protects the deeper layers of the skin from UV damage from the sun. Although people of color are less likely to become afflicted with skin cancer, they are much more likely to die from it due to delayed detection.
Treatment.
No two skin cancer patients are the same, and the recommended treatment for each individual varies. Treatment for skin cancer depends upon the following factors:
- type of skin cancer
- location
- age and overall health of the patient
- size of the cancer
- cancer stage
- possible side effects of treatment
After a healthcare team considers the following factors, they may recommend one or more of the following treatments:
- Cryotherapy. Liquid nitrogen is used to freeze off the cancer cells, and the dead cells are cast off after treatment. This method effectively treats early cancers in actinic keratosis or other precancerous skin lesions.
- Excisional therapy. The tumor and surrounding cancer cells are cut out and removed.
- Mohs therapy. The raised area of the tumor is removed first. It is then removed layer by layer under a microscope under no more cancerous cells are visible.
- Curettage and electrodessication. A tool with a looped edge is used to scrape off cancer cells, and the area is then treated with an electric needle to destroy the remaining cells.
- Chemotherapy. Anticancer medications are applied topically if the cancer is limited to the skin’s top layer. If the tumor has spread to other parts of the body, medication is provided through pills or IV.
- Immunotherapy. Certain medications are used to stimulate your immune system to act against cancer cells.
- Radiation therapy. High energy waves like x-rays, gamma rays, electron beams, or photons are used to destroy the cancer cells.
- Photodynamic therapy. The skin is coated with medication, and fluorescent light is used to activate the medication. This destroys precancerous cells while leaving normal cells alone.
Cancers are generally treated by dermatologists. Depending on its stage, however, it may be treated by another type of doctor, like:
- surgical oncologist (surgical treatment)
- medical oncologist (chemotherapy, immunotherapy, and other medication-based treatments)
- radiation oncologist (radiation therapy)
It is important to think over your options for treatment by giving yourself some time to think. It is also important to clear any concerns of yours with a medical professional.
Complications.
The most common complications of skin cancer include:
- Metastasis. When the cancer cells spread from your skin to other parts of the body.
- Scarring. Treating basal cell and squamous cell carcinomas can leave behind scars, depending upon the type of treatment and other factors.
- Lymphedema. When the cancer cells spread to your lymph nodes, your arms and legs can well up due to the damage.
- Hematoma. This is the bleeding under the surface of the skin, caused when a mass formed puts pressure on a wound.
- Damage to muscles, nerves, and bones. If left untreated for too long, skin cancers can grow deep enough to cause damage to the muscles and bones.
Skin cancers can be more or less complicated based on their type, location, and size among other factors. The health of the patient also plays an important role in treatment. You are also at a heightened risk of developing cancer again if you had it previously, with many cancers returning within 5 years of treatment.
Can you prevent skin cancer?
Prevention of skin cancer requires extensive attention to protection from the sun’s damaging UV rays, especially for extended periods. Ultraviolet rays cause DNA damage and genetic mutations in your skin cells, which leads to skin cancer.
The following tips can reduce your risk of skin cancer:
- Wear sun-protective clothing. Long-sleeved shirts, pants, and wide-brimmed hats. Clothing with an ultraviolet protection factor (UPF) is more effective in protecting from the sun’s damaging rays.
- Apply broad-spectrum sunscreen (SPF 30 or higher). SPF stands for Sun Protection Factor. It tells you how long the sunscreen could protect you from the sun’s UVB rays. For example, it would take you 30 times longer to burn with an SPF 30 product than if you used no sunscreen.
- Reapplication. No matter the SPF of your sunscreen, reapplication every two hours is key. Sunscreen must also be reapplied after sweating or swimming, even if it’s water-resistant.
- Wear sunglasses. Sunglasses that offer 100 percent UV protection are the most effective.
- Avoid direct sunlight. Avoiding sun exposure, especially during peak hours of 10 a.m. to 4 p.m., by seeking shade or staying indoors.
- Avoid tanning beds. The ultraviolet rays from tanning beds are a common cause of skin cancer and premature aging of the skin.
- Cloudy days are not safe. Even when it’s cloudy outside, up to 80 percent of the sun’s damaging UV radiation reaches the skin. Therefore, you should not avoid your skin protection ritual even on cloudy days.
Regular examinations from a dermatologist are key in reducing this risk. You can also have someone in your family examine your skin for any unusual changes, especially in areas not clearly visible, like the back.