The Lamen
Researchers find specific long COVID biomarkers in blood of patients
Long COVID has been confusing to deal with, for patients and physicians alike. The lack of a means of diagnosis has largely kept things at a standstill. New research, however, looks to change the playfield through blood tests.
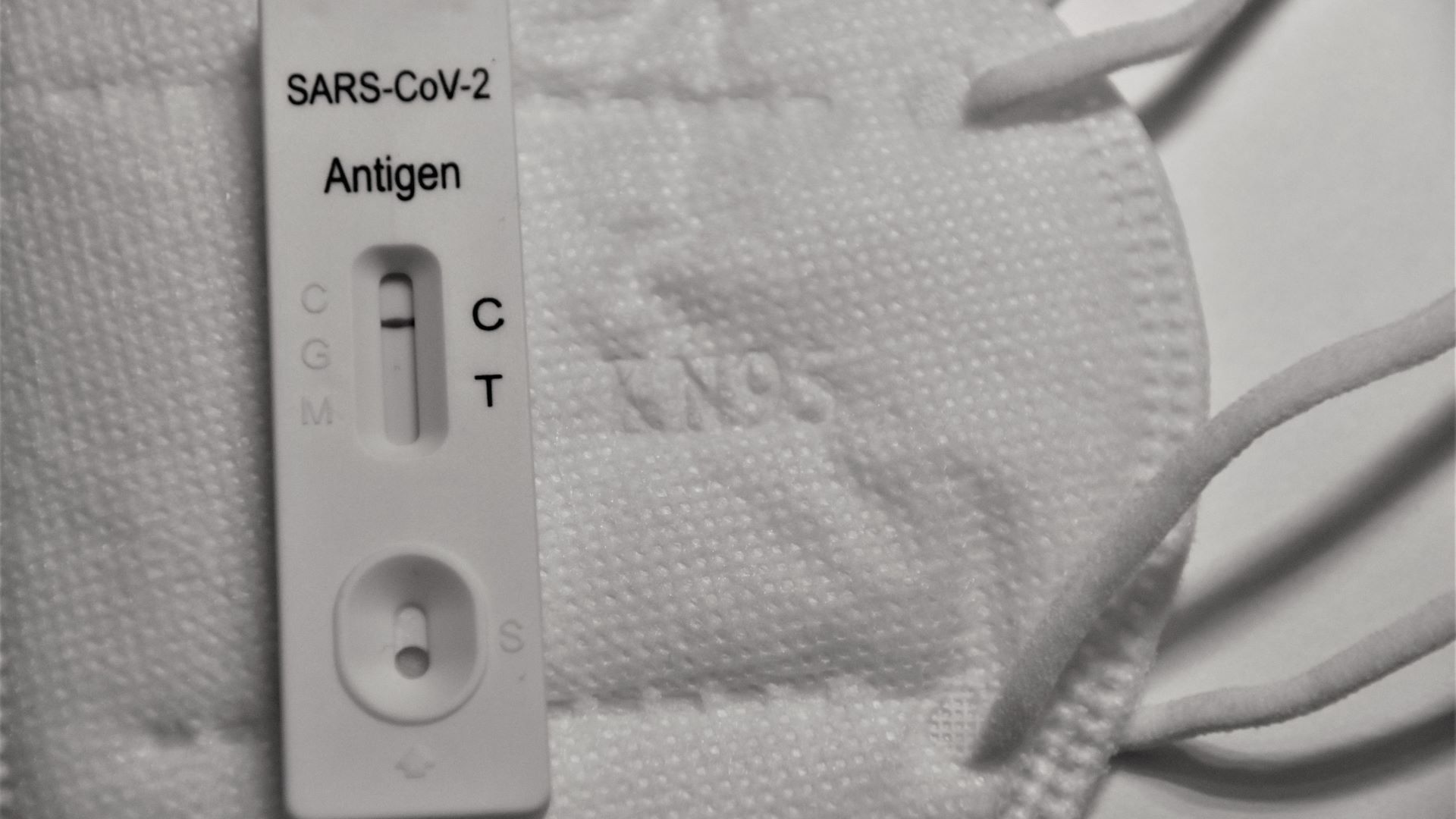
Photo: Unsplash
Disentangling the symptoms of long COVID from those of other chronic conditions has been a head-scratcher — one that has spawned thousands of studies over a few years. Research has been confusing and contradictory at times, having millions dealing with symptoms that often go unacknowledged.
Scientists take a “decisive step” toward long COVID detection as they find identifiable biomarkers in the blood
Explainer: Understanding this hot mess of disabling symptoms has made scientists look to the blood — who have found identifiable biomarkers in a “decisive step” toward long COVID detection.
- Initially posted as a preprint last year, the study published in Nature compared people with active long COVID symptoms at least 4 months after initial COVID-19 infection to those with no COVID-19 infection and those who had fully recovered from a confirmed case of COVID-19.
- After a self-reported questionnaire about symptoms and health-related quality of life, researchers took blood samples from the patients — using a machine-learning algorithm to detect differences.
They found that people with long COVID had:
- abnormal immune cell levels
- reactivation of multiple dormant viruses, like the Epstein-Barr virus
- significantly reduced levels of cortisol, a stress hormone that controls inflammation, regulates blood pressure, and influences the sleep/wake cycle
However, these biomarkers can be highly variable among patients, requiring physicians to adopt a highly personalized approach to detection accounting for medical histories.
The researchers said that this study “is one of the first to show us clear, measurable differences in blood biomarkers of people with long COVID compared with people who recovered fully from an acute infection,” adding that “this is a decisive step forward in the development of valid and reliable blood testing protocols for long COVID.”
False negatives and varying symptoms make detection all the more confusing
Long COVID is estimated to occur in at least 10 to 20 percent of COVID-19 cases, but the figures have been all over the place — owing to detection discrepancies.
A group of 10,000 participants recently described 12 symptoms that “best differentiated” a long COVID infection, including fatigue, brain fog, and gastrointestinal symptoms — but detection continues to evade many.
- Long COVID has been associated with over 200 symptoms, many overlapping with common conditions like the flu.
- The lack of an agreed-upon definition, no clearly detectable features to aid diagnosis, and the presence of varying phenotypes have made guidelines tough to assign.
Meanwhile: The NIH’s Recover initiative has already launched several clinical trials in efforts to “rapidly improve our understanding of and ability to predict, treat, and prevent PASC, including long COVID.”